Discover if it is safe for your workers to be taking medicinal cannabis.
Read more
Registered medical practitioners in Queensland can now prescribe medicinal cannabis to their patients if they think it’s clinically appropriate. Previously, only specialist doctors had the authority to issue such prescriptions. But a recent amendment to existing legislation effectively changed this requirement.
With more doctors allowed to issue medicinal cannabis prescription, it raises new concerns for the public. Is it safe for workers to use the drug? Will it affect their performance at work? Here’s our take on the matter.

Medicinal cannabis use in Australia
In 2016, the Australian government legalised the use of medicinal cannabis at the federal level.
Since then, doctors have used to treat a number of medical illnesses. These include epilepsy, multiple sclerosis (MS), and non-cancer chronic pain.
Researchers have also tried using medicinal cannabis to treat nausea and vomiting due to chemotherapy and for palliative care.
However, the government heavily regulates access to medicinal cannabis under the Therapeutic Goods Act (TGA) of 1989. Only health professionals with Commonwealth approval could obtain the drug for treatment purposes.
Each state has its own restrictions regarding the production and sale of medicinal cannabis. But the general rule applies that no private individual can obtain their own supply of the drug.

Queensland’s new medicinal cannabis legislation
In April 2020, Queensland lawmakers passed a new law to help simplify the medicinal cannabis prescription process. They now classify the drug as Schedule 8 medicines (drugs of addiction) or Schedule 4 medicines (prescription drugs).
The law now allows doctors in the state to prescribe medical marijuana to patients with any condition. Meanwhile, non-specialist medical practitioners will still need state approval to prescribe Schedule 8 medicinal cannabis.
Queensland’s Minister for Health and Ambulance Services, welcomed the passing of the new law. However, some health professionals have expressed their concern about the simplification of the prescription process. They prefer that doctors and patients still explore other avenues first before considering the use of medicinal cannabis.
Doctors have to consider the potential dangers of medicinal cannabis abuse. If the drugs were to become more readily available, it could increase people’s risk for driving impairment.
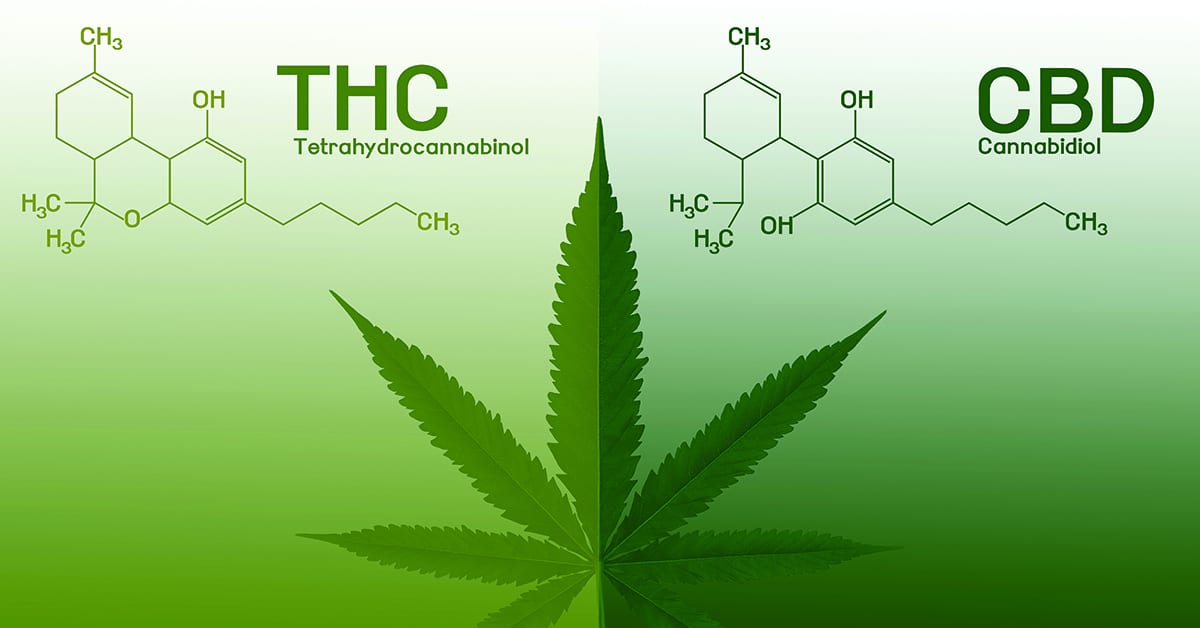
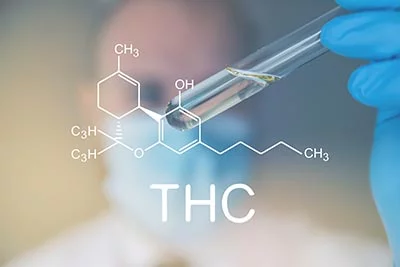
We also have to take a closer at the effectiveness of such medications. There should be a clear distinction between medicinal CBD (cannabidiol) and (tetrahydrocannabinol) THC. This is very important since CBD has no substantive impairing effects unlike THC.

Medicinal CBD vs THC
CBD and THC are two of the substances extracted from cannabis. While these cannabinoids have similar chemical structures, they don’t have the same psychoactive effects. For instance, CBD doesn’t produce the same level of high or euphoric effects that THC does.
Both cannabinoids also have different ways of affecting the human brain. THC binds with the cannabinoid 1 (CB1) receptors, which triggers the release of dopamine. This causes a feeling of high or euphoria. It also leads to the performance impairment often experienced by users
Meanwhile, CBD primarily affects CB2 receptors. When bound, these receptors don’t release dopamine. However, they do help reduce inflammation, nausea, and neuropathic pain.
CBD can also bind with CB1 receptors but only very weakly. You need to pair CBD with THC before it can properly bind with a CB1 receptor. This will help reduce some of the psychoactive effects of THC such as sedation or euphoria.
Side effects
CBD is considered to be the compound more tolerated by the body, even in large doses. Its known side effects include dizziness, fatigue, appetite changes, weight loss, and diarrhea.
On the other hand, THC causes temporary side effects such as red eyes, dry mouth, increased heart rate, anxiety, and slower reaction times. It can also result in memory loss and coordination problems.
Both CBD and THC can cause psychoactive effects on users. These side effects are not considered fatal, but they can affect an individual’s health and well-being.

Impairment
Medicinal cannabis is considered safe, as long as patients take CBD alone. Combining CBD with THC or any other sedative can already lead to adverse effects.
In 2019, Arkell et al examined the impact of cannabis-based medication on 14 individuals. The participants used drugs that contained both cannabidiol and THC.
The researchers made the following observations:
- Substantial impairment lasted for more than 4 hours after using cannabis-based drugs.
- When driving, participants were more susceptible to lane weaving and had slower attention focusing.
- Participants compensated for their ‘stone’ condition by reducing their speed and maintaining safe car spacing. However, they are still more likely to lane weave.
- Drivers who used a combination of CBD and THC performed worse than those that did not.
Many cannabis users claim they are safer drivers than alcohol users. This isn’t necessarily the case. Stoned drivers will try to compensate for their condition. However, it doesn’t change the fact that they’re still likely to drive unsafely.

Drug testing
Drug driving laws pertaining to cannabis aren’t as clear-cut as many would like. For example, in New South Wales users can lawfully drive as long as they are not impaired. However, this places the burden of determining the capacity to drive and level of impairment on the prescribing doctor. They need to have a firm understanding of the drug’s effects on their patient.
On the other hand, the Road Transport Act of 2013 states that driving with any detectable amount of THC is against the law. This is consistent with all other state laws, including Queensland. The law doesn’t include any exclusions for prescribed medicines.
What does this mean for medical marijuana users? If you’re using true CBD oil without any sedatives, you have nothing to worry about. Pure CBD oils aren’t detectable through drug testing. You have to be careful though since many dubious CBD oil products contain some amounts of THC. Some of these products even contain only cannabis extracts in coconut oil.
Meanwhile, THC medications have the same detection window as for smoked cannabis. THC is detectable via urine testing for up to 72 hours. However, this time frame doesn’t correlate with the one needed to establish a person’s impairment.
Oral fluid testing offers a better way of determining impairment. Saliva analysis can detect THC between 8 to 24 hours, depending on the dose. If a person tests negative via oral fluid, then they are assumed to be unaffected by impairment.
Safety concern
It’s highly important to determine the exact level of impairment among workers, especially those working in safety-critical industries. Most individuals claim to be unimpaired because they no longer feel stoned. But this doesn’t necessarily mean that they are safe to perform their usual complex tasks.
While taking medicinal CBD alone is considered safe, users still need to be careful. If they mix the drug with THC or any other sedative, it could result in serious impairment.
Watch our webinar on medicinal cannabis use below to know more about medicinal cannabis use:
Learn More
Contact us today to learn how we can help you with your workplace drug and alcohol testing needs.
A quick and simple guide on how to spot tell-tale signs of drug abuse in your workers.
Read more
As a business leader, you need to keep an eye out for signs of drug use in your workplace. But looking after the health and safety of your employees can be a real challenge. You need to have a reliable system of identifying evidence of drug abuse and how to properly address it.
Here’s our quick and simple guide on how to spot tell-tale signs of drug abuse in your workers.
How to spot signs of drug use in your workers
Before you start checking everyone in your company, there are a couple of things you have to remember. Unless you’re a medically-trained professional, you won’t be able to fully diagnose a person for drug addiction. You can only identify certain patterns of behaviour in your employees that could suggest potential drug use.
There’s also the possibility that some of the symptoms you may find are linked to other health conditions. That’s why it’s important that you create a proper action plan before you act on your suspicions. It doesn’t hurt to always be careful.

Marijuana use
National wastewater analysis shows that marijuana (cannabis) is one of the most commonly used drugs in Australia. This might be because of how easier it is for Aussies to obtain the drug compared to other controlled substances. However, new evidence suggests that cannabis consumption throughout the country may actually be dropping.
The health impact of marijuana use comes from the plant’s main psychoactive ingredient: THC. The substance stimulates a person’s brain much like food or sex. It triggers the release of dopamine, which helps the user feel relaxed or even euphoric.
People who use marijuana often experience the following physical and behavioural effects:
- Red eyes
- Faster heart rate
- Poor muscle coordination
- Delayed reaction times
- Increased appetite
Cannabis use can also cause people to abruptly change moods. They could go from being extremely tense one moment and then become super relaxed the next. In some cases, users can suffer a sudden onset of anxiety, panic, and/or hallucinations as well.
Other tell-tale signs of marijuana use include:
- Sleepiness
- Lethargy
- Lack of focus
- Talkativeness
- Misjudgment of time
- Secretiveness

Alcohol use
Alcohol is another popular mood-altering substance. It’s not unusual for Aussies to enjoy a few drinks, especially after a hard day’s work. But sometimes their attraction to alcohol can go out of hand. Some workers report to work intoxicated after a night of drinking, while others even do their drinking in the office.
Keep a lookout for these signs to find out if your employee is suffering from alcohol use or addiction:
- Bloodshot eyes
- Unkempt appearance
- Smell of alcohol on breath and skin
Inebriated workers also show several odd behaviours, including:
- Sleeping on duty
- Sluggishness
- Experiencing tremors
- Temper outbursts
- Irrational or aggressive behaviour
Additionally, those who abuse alcohol are more likely to come to work late or skip workdays entirely.

Cocaine use
Cocaine can cause far-reaching health consequences, especially when used for long periods. The drug triggers an intense but short-lived high in users followed by an equally intense bout of depression and edginess.
People who abuse cocaine often have to take increasing amounts of dope to get high. This causes them to become more addicted to the drug. Symptoms of cocaine use include:
- Dilated pupils
- Runny nose
- Burned lips or fingers due to smoking cocaine
- Track marks from injecting cocaine
- Damaged nasal passages due to snorting cocaine
You might also see some erratic behaviour from someone who uses cocaine, such as:
- Nervousness
- Restlessness
- Talkativeness
- Irritability
- Anxiety
- Restlessness
- Aggressive behaviour
- Feeling of superiority toward others
- Paranoia

Methamphetamine use
Like cocaine, meth (ice) can produce severe physical and psychological effects on long-term users. The drug chemically alters how a person thinks or feels, which could result in significant behavioural changes. Some of the most common physical signs of meth use or addiction include:
- Dilated pupils
- Skin sores
- Rotting teeth
- Extreme weight loss
- Burns, particularly on the lips or fingers
Meanwhile, meth abusers also show noticeable erratic behaviours, such as:
- Hyperactivity
- Agitation
- Paranoia
- Rapid eye movement
- Reduced appetite
- Erratic sleeping patterns
- Mood swings
- Twitching, facial tics, or jerky movements

Heroin use
Believe it or not, not all heroin addicts get their start by abusing the drug immediately. Some people use heroin as a stronger and more affordable alternative to prescription painkillers like oxycodone and hydrocodone. But the potency of the drug only ends up stoking their addiction.
Heroin abusers often show the following symptoms:
- Bloodshot eyes
- Constricted “pinpoint” pupils
- Sudden weight loss
You might also notice the person experiencing sudden behavioural changes, including:
- Lack of motivation
- Secretive behavior
- Extreme drowsiness or nodding off at work
- Financial problems
Learn More
Your workers are the backbone of your business. That’s why it’s important that you’re aware of their health and well-being. If you suspect anyone in your organisation is suffering from substance abuse, it’s best to act now and intervene. The safety of your employee and the future of your company may depend on it.
For help in conducting drug and alcohol testing at the workplace, contact us today.
Learn about benzos and how they affect workers health and safety.
Read more
Australia has a long history of battling benzodiazepines abuse dating back to the 1970s.
While the government was successful in controlling the supply of the drugs, it ultimately failed in stopping the demand. Regulatory measures only forced the drug trade underground, giving birth to a thriving and lucrative black market.
Today, ‘benzos’ continue to fuel Aussies’ addiction to prescription drugs with no clear end in sight.
What exactly are benzodiazepines and how can they affect workers’ health and well-being? Our chief toxicologist Dr Phil Tynan breaks down the history and profile of these psychoactive drugs.

The (unwelcomed) return of an old friend
What are benzodiazepines?
Benzodiazepines (BZOs) are a group of drugs that treat anxiety and insomnia. During the 1950s, doctors used barbiturates to treat patients with anxiety disorders. However, researchers found out that these depressants were highly addictive and fatal in high doses.
In 1960, Swiss pharmaceutical company Roche released the first of its benzodiazepine-class drugs. Compared to barbiturates, benzos proved to be a much safer option at treating anxiety disorders. The discovery helped propel benzodiazepines to prominence. In fact, Valium—a common BZO—became the most prescribed drug in the U.S. by 1968.
Unfortunately, the early enthusiasm for benzodiazepines was somewhat misplaced. Benzodiazepines turned out to be just as addictive to patients as barbiturates. The psychoactive effects remain even for continuous use of 3 to 4 weeks.
Benzo abuse can also result in serious health conditions for users. Unmanaged withdrawal can lead to life threatening crises associated with severe fitting. Meanwhile, mixing BZOs with alcohol or opiates increases the risk of fatal overdoses.
Despite these health risks, benzodiazepine use still has its benefits. Benzos play a legitimate role in helping patients deal with insomnia in the short term. They are also used as potent anti-seizure agents and as treatment options for alcohol withdrawal.
These days, doctors still rely on benzodiazepines to treat patients suffering from panic attacks and generalised anxiety disorders.
Government stops over-prescriptions to curb benzodiazepine addiction
BZO addiction was originally a result of overprescription. The Australian government tried to put a stop to this by enforcing stricter prescribing controls. In 2011, the number of benzodiazepines prescriptions dropped by 24.9% from its peak in 1992.
However, Australians had merely switched from one form of benzodiazepine to another. They traded Valium for Alprazolam, which is more commonly known as Xanax. This led to a doubling in prescription rates from 2000 to 2010.
To combat this, the government named Xanax as a controlled drug. By restricting BZO prescriptions, authorities believed it would help prevent doctors from over-prescribing and onselling the drugs. It would also discourage patients from ‘doctors shopping’, or seeing multiple treatment providers to get medical prescriptions illicitly. The government hoped to stop the diversion of medical BZOs.
At first, these regulatory efforts seemed to have worked. The country saw a noticeable decrease in benzodiazepine use. However, this gave way to a new wave of BZOs hit.
The problem resurfaces with benzo analogues in the black market
Instead of diverting benzos from medical supplies, smugglers have resorted to selling ‘pressed’ versions of the drugs. Pressed BZOs are drugs that were turned into liquid or powder. Drug makers then cut and press these substances into pills and sell them as knockoffs on the streets.
To make matters worse, drug dealers are now selling new analogues of current BZOs. They have nearly-identical drug molecules and mostly similar effects with known benzodiazepines. However, Australian laws do not cover these new benzo analogues.
One example is Flubromazolam, which is an analogue of Valium. This drug is 10 times more potent than Xanax and can cause serious harm to users.
Benzodiazepines abuse in the workplace
Benzodiazepine abuse can often lead to workplace accidents. Workers who use the drugs can experience an 81% post-usage impairment when performing complex tasks, especially spatio-temporal tasks.
Benzo use significantly impairs working memory and limits the ability to pay attention. It also prevents proper risk-assessment since the drugs tend to block a person’s ability to worry.
Urine benzodiazepine test
Urine tests are a more effective way of drug testing for benzodiazepine use than oral fluid tests.
Only a small amount of BZOs make it to oral fluid specimens, causing oral fluid tests to miss the presence of the drugs.
Benzos also have almost the same detection window and impairment period. However, some of the new analogues are more difficult to detect and can only be assayed during a laboratory drug test.
Stopping benzodiazepines abuse may not be as simple as cutting off drug supplies. As long as there’s a significant demand for the drugs, people will find a way to get their benzo fix.
One way to address the issue is by raising awareness on the dangers of BZO dependence. It is recommended that workplaces implement a drug and alcohol education and training program.
By letting people know how benzodiazepines can damage their health, they’ll be more keen on avoiding them.
Learn More
Your workers are the backbone of your business. That’s why it’s important that you’re aware of their health and well-being.
If you suspect anyone in your organisation is suffering from substance abuse, it’s best to act now and intervene. The safety of your employee and the future of your company may depend on it.
For help in conducting drug and alcohol testing at the workplace, contact us today.
New guidelines for the collection of samples for an oral fluid drug test.
Read more
Standards Australia and Standards New Zealand have come out with new guidelines regarding the collection of samples for an oral fluid drug test. Designated as AS/NZS 4760:2019, the standard outlines several changes to the requirements for accredited screening for signs of drug abuse found in saliva specimens.
Read on to learn more about the new oral fluid standard. Find out how it is going to affect Safework Health’s drug screening service for its clients.
What is AS/NZS 4760:2019?
As with any new standard in workplace drug testing, the change to the new requirements will evolve over the coming months as device manufacturers, on-site testing providers, regulatory bodies and others respond to the updated standard.
There are a number of significant as well as minor changes required to how an on-site saliva test for drugs of abuse is tested, collected, transported and analysed in a laboratory.
Changes to the collection procedure for an oral fluid drug test
A. Donor Informed consent
Drug testing companies should inform donors of the procedure for addressing disputed results. The expansion of collection procedures requires collectors to do the following:
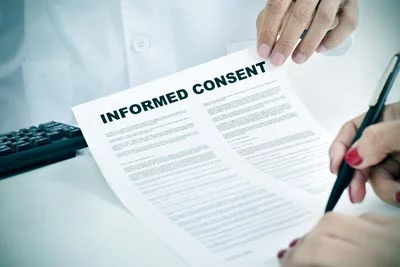
- Verbally obtain full consent from the donor
- Explain the privacy requirements covering the sample and its analysis
- Report and inform the donor about procedures covering disputed results
Testing companies should also include these changes in their Collector training program.
B. Tamper evident seals
If a donor places their initials on the seal of their test sample, they also have to put their initials on the Chain-of-Custody form.
Safework Health already requires donors to place their initials on seals and sign the Chain-of-Custody form. There won’t be any major changes to its existing procedures.
Modifications to the Chain of Custody form
Under AS/NZS 4760:2019, the Chain-of-Custody form should feature additional items. This includes the expanded donor informed consent and recording transport device.
Changes to on-site oral fluid drug test procedures
A. New screening cut-off levels
AS/NZS 4760:2019 sets new cut-off levels for substances identified during drug screening.
- THC screening cut-off is now down to 15 ng/mL from the initial 25 ng/mL
- Oxycodone levels now has a cut-off of only 40 ng/mL
The National Association of Testing Authorities (NATA) said it expects new screening devices will become available within a year of the current date. In the meantime, the agency encourages drug testing companies to still use their existing screening devices.
Meanwhile, Safework Health is currently testing new and upgraded versions of screening devices. We will have instant (onsite) drug testing devices compliant with the new standard ready within the next 3 to 4 months.
Our team will inform our clients as soon as the devices become available.
B. Verification
The new standard requires drug testing companies to verify their sample transport devices. For our part, Safework Health already verifies its existing devices, such as Quantisal.
Changes to the reporting of oral fluid drug test results
A. Reportable cut-offs
Standards Australia and Standards New Zealand has updated its guidelines for reportable cut-offs involving an oral fluid drug test.
THC
AS/NZS 4760:2019 reduces the reportable cut-off for THC screening tests from 25 ng/mL to 15 ng/mL. It also lowers the threshold for confirmatory tests from 10 ng/mL to 5ng/mL. However, both moves have raised significant concerns regarding the potential impact of passive cannabis smoking.

Niedbala et al report (2004 and 2005)
In 2004, researcher Niedbala and colleagues reported levels of THC in oral fluid up to 4.2 ng/ml in reasonably ventilated environments.
However, in the presence of regular (i.e, non-extreme) cannabis smokers in very poorly ventilated environments, OF THC levels were substantially higher. The study recorded oral fluid THC levels ranging from 3.6 ng/mL to 26.4 ng/mL.
A subsequent study also by Niedbala et al. in 2005 found oral fluid THC levels between 3ng/mL and 14 ng/mL. The researchers saw this in cases of passive smoking in normally ventilated rooms within 2 hours of testing.
Cone et al report (2015)
In 2015, Cone and fellow researchers came across similar findings to those of Niedbala et al.
In their own report involving an average OF THC 6 passive subjects, Cone et al found that all passive THC exposures were undetectable 75 to 90 minutes after use. They came across the result regardless of the subjects’ exposure levels.
One can derive a 90 minute to 2 hours limit for potential passive cannabis exposure. Any collection after this period would be ascribed to active use of the substance. Concerns regarding passive smoking can therefore be negated.
Screening OF THC cut-off at 15 ng/mL
The process may be able to capture some passive smokers only if they are:
- Exposed to high [THC] cigarettes ~ 11.3% Δ 9 -THC.
- Staying in a very poorly ventilated environment NOT a standard room.
- Tested after 90 to 120 mins of exposure or if they are in a THC contaminated room.
Confirmatory OF THC Cut-off at 5 ng/mL
The process may capture passive smokers if they are:
- Staying in a poorly ventilated environment.
- Tested within ~ 3.5 hrs of exposure or if they are in a THC contaminated environment.
These guidelines will not be applied under any other circumstances.

Cocaine metabolite Ecgonine methylester (EME)
Standards Australia and Standards New Zealand have removed cocaine metabolite EME from their list of reportable substances.
Safework Health will continue to assay EME in its reports. We will flag test results that will show abnormal ratios of cocaine metabolite since these may have a bearing on the time of use.
Oxycodone
The updated standard formally establishes the cut-off level for oxycodone at 20 ng/mL.
B. Format change
All reports should clearly specify that the security seals for specimens are intact. The statement effectively replaces the practice of appending ‘CoC complete’ on collected samples.
Collectors need to record the devices used for OF collection, transport and storage (e.g. Quantisal).
Testing reports will now use AS/NZS 4760-2019 as their concluding standard reference.
Guidelines regarding disputed results
Standards Australia and Standards New Zealand have set guidelines in cases where there is a disputed result. Drug testing companies are required to do the following:
- Recommend replicate analyses
- Obtain the Donor’s consent before they send disputed results for reanalysis.
- Issue disputed results to the donor, the requesting authority and to the laboratory that originally tested the sample in question.

Criteria for rejection of oral fluid drug test samples
AS/NZS 4760-2019 provides new criteria for rejecting test samples.
For instance, the Chain-of-Custody form cannot be corrected for fatal errors. This includes wrong name or ID, incomplete form, and incomplete or unlabelled specimens.
In case there is a rejected sample, Safework Health will still issue the results. However, the subsequent report will have to specify that the Chain-of-Custody was not intact.
A non-intact Chain-of-Custody is not considered viable evidence in a Court of Law.
Changes in the designation of Collectors
Standards Australia and Standards New Zealand define a Collector as someone who has successfully completed training for the following:
- Oral fluid collection
- On-site drug screening (if applicable)
- Handling, storage and dispatch of specimens
A Collector also needs to show that they are competent in executing their duties.
NOTE: Courses for Collectors may be provided by the Vocational Education and Training (VET) Quality Framework, the Faculty of Clinical Forensic Medicine (RCPA), the New Zealand Qualification Authority. This also includes programs that offer equivalent training.
Safework Health provides our own accredited training courses for oral fluid collectors.
Safework Health’s Adoption of AS/NZS 4760-2019
Safework Health has begun introducing the new guidelines established with AS/NZS 4760-2019. We started adopting the new guideline in October 2019. Our team is working with clients to help familiarise them with the changes.
If you have questions or want to discuss AS/NZS 4760-2019 more in depth, feel free to contact us today.
You can also buy a copy of the new Standards Australia or Standards New Zealand guideline HERE.
References:
- Niedbala et al J Anal Toxicol. 2004 Oct;28(7):546-52
- Niedbala et al. J Anal Toxicol, 2005 Oct;29: 607-15) .
- Cone et al J Anal Toxicol 2015 Jan; 39(1):1–12
Learn what to do if your employee refuses a drug test.
Read more
So your employee has refused a drug test. You are probably thinking — is this even possible?
You’ve seen the figures: employee drug and alcohol use costs Australian businesses $6 billion per year in lost productivity.
As an employer, you have every right to perform drug and alcohol testing. This is true not just in high-risk industries such as construction, mining, transportation and aviation, but in all industries across Australia.
Beyond the already stated financial losses, it is your legal obligation to provide a safe and healthy work environment for your employees.
Especially when you consider the effects of drug and alcohol use at work — lack of focus, poor concentration, aggression, unstable moods, lack of coordination, and unwanted sexual advances.
Clearly none of us wants an employee to exhibit these highly inappropriate behaviours. We also don’t want anyone else on our team to experience such bad behaviours from their coworker.
What To Do If An Employee Refuses To Be Tested
Legally, speaking, you cannot force an employee to undergo a test if it’s against their will. Doing so could lead to civil liability.
Trying to reason or threaten your employee will rarely have any positive results. At best you’ll get a definitive ‘no’ from your worker. At worst you’ll cause a revolt and outright destruction in your entire team.
It is best to stick to well established rules and procedures. This is where a well-written and clearly-worded drug and alcohol policy comes in.
David Dilger, an employment and safety lawyer at Edge Legal, believes companies could insist on drug testing as part of employment as long as it is reasonable.
Workers don’t necessarily have to see any mentions of an alcohol and other drugs policy in their contract. They could find something like ‘you’ll comply with our policies and procedures as lawful and reasonable direction’.
An employee has to comply to a workplace drug test, provided that it is a lawful and reasonable direction, Dilger expplained. If they were to refuse, they could face disciplinary action and might even lose their job.
In some cases, a worker can get fired not because they failed a drug test but because a court or tribunal found them to be non-compliant with a reasonable policy.
Dilger added that more modern alcohol and other drugs policies prioritise work health and safety rather than penalising employees.
Workers who refuse to participate in drug testing could be considered in breach of their duty. Their employers might take their refusal to be going against a policy meant to ensure the safety of their workplace.

Review Your Drug and Alcohol Company Policy
As an employer, your workplace drug and alcohol policy must indicate clearly the reasons for subjecting an employee to a drug test. For instance, the improvement of productivity, the safety of the operations, and maintaining good health.
You have to make sure that your policy also specifies the consequences a worker might face if they were to refuse testing.
Every employee should have signed the workplace drug and alcohol policy, understanding and agreeing to a drug test for justifiable reasons.
In Australia, it is perfectly legal to conduct workplace drug testing at work. However, crucial to effectively enforcing it is establishing a workplace drug and alcohol policy beforehand.
Why? Because it is important that your employees are aware of the following:
- Reason for drug tests
- Who will do the testing
- Drug testing schedules
- How often the drug test will be carried out
- Drug test types
- Accepted blood alcohol limits
- What to do in the event an employee tests positive for drugs or exceeds accepted limit for alcohol
- Disciplinary measures for employees who will refuse to be tested
This is legally the only way to go about drug testing. The methods, frequency and consequences must be clearly stated. Every employee should be fully aware of these guidelines. Meanwhile, as an employer, you have to follow all of the things you’ve outlined in your drug and alcohol policy.
Similarly, if you update your processes, you must reflect the changes in your policy, inform everyone affected and have proof you have done so.
What If I Do Not Have A Legally Binding Workplace Drug And Alcohol Policy?
If you do not have a sound drug testing framework for your workplace, you simply cannot enforce any kind of drug testing. Even if an employee tested positive, you would likely not be able to apply any kind of consequences.
One of the best ways to do this is by teaming up with an experienced workplace drug and alcohol testing provider.
Having a capable and reliable drug testing partner can help protect your company from liabilities related to workplace substance abuse. It can also make your workers feel more comfortable and trusting of your policy.

Drug and Alcohol Testing at Work
Safework Health will help you safeguard your business and employees from drug and alcohol-related incidents at work.
We will help create a comprehensive drug and alcohol policy for your company that includes:
- staff training
- drug awareness programs
- drug and alcohol testing
Moreover, our fast turnaround times for drug testing results mean minimal downtime on your operations.
Whatever your circumstances, contact us today for a confidential discussion.
Learn about drug abuse in white-collar professions in Australia.
Read more
When thinking of a drug addict, most people picture someone lowly educated and living off crime. However, in Australia, the profile of a drug abuser challenges these stereotypes.
In our country, drug abuse is a problem not exclusive to unemployed or low skilled workers. In fact, there is one sector that is contributing to Australia’s steadily growing drug problem — the white collar professionals. The typical drug user in Australia is a professional with tertiary education.
A report by the National Drug Strategy Household Survey confirms this: a majority of cocaine users are between the ages of 20-39, educated, employed, and living in major cities. In addition, they also belong to the highest socioeconomic status. As Will Tregoning — founder of a non-profit organisation committed to challenging current drug policies — once said: “A lot of wealthy people take drugs.”
Read on to find out the incredible truth about drug abuse in white-collar professions in Australia.
A high stakes job puts the pressure on professionals. Long working hours, an intense social scene, plus a large disposable income create the perfect context for drug abuse.

Most Affluent Suburbs Are The Biggest Consumers of Cocaine
Drug abuse is interwoven into the corporate culture of Sydney. And one drug — cocaine — is proving to be the substance of choice of Australia’s wealthiest and most influential in the country. The number of cocaine users continues to grow among C-level professionals who work in the banking, legal, and finance industry. Many state that obtaining the drug is very easy.
In 2016, the Daily Telegraph accessed court documents detailing the operations of a drug syndicate in Sydney. Shockingly, a 64-year-old suburban grandmother headed the family-run drug syndicate. They admitted to peddling 30 bags of cocaine a night. Distributing the lot to their high-flying clients in Sydney’s northern and eastern suburbs. Furthermore, Sydney police also note a steady increase in drug-related incidents in Sydney’s wealthiest suburbs around the same time.
The Oceania market for drugs is extremely lucrative according to the 2014 United Nations World Drug Report. In fact, the most powerful drug trafficker in the world, Sinaloa Cartel kingpin “El Chapo” established a cocaine importation business on the eastern part of Australia. In 2015 Police intercepted a shipment by the cartel of 240kg of cocaine, worth about $83 million in Sydney. The monthly consumption of cocaine across the Australian east coast is about 500 kilograms a month.
The Easy Slide into Cocaine Abuse
Dr. Christian Rowan, Addiction Specialist at The Banyans Health and Wellness Residence says cocaine use is popular due to its stimulating effects. On it, the user is wide awake and buzzed on energy. Two major reasons for using it are to stay awake and alert for work and to unwind and relax for socialising.
Cocaine users also prefer the drug because of its very few physical symptoms. With less obvious symptoms, social users can shrug it off as a harmless habit. Being high on cocaine may not as obvious as being high on marijuana, but that’s what makes the drug so insidious. Because the negative effects of cocaine develop gradually and are not immediately noticeable, it is particularly dangerous.
Because of its high cost and the class of people who use it, cocaine has also become a status symbol. There is a sense of glamour to using cocaine and being one with the elite. What’s interesting is how cocaine users do not consider themselves addicts, referring to themselves as “recreational” users.
Misconceptions About Cocaine
Another factor that adds to the growing number of cocaine users is the misconception that cocaine is not as dangerous as other drugs. Since early users of cocaine are introduced to it socially, it makes the drug seem harmless. Furthermore, the social context makes them unaware of their developing drug dependency. However, socially driven cocaine use is highly dangerous.
The findings, published in the medical journal PLOS ONE show that cocaine users have increased aortic stiffness, greater left ventricular mass, and higher systolic blood pressure. According to Professor Gemma Figtree of Sydney Medical School, there are acute side effects of cocaine use. Some of which include myocardial infarction or heart attack. Cocaine users often use it in conjunction with alcohol, which is harmful to their health.
Cardiovascular disease is the leading cause of death in Australia. And men who suffer from heart disease are getting younger and younger. Could growing cocaine use in the country have something to do with it?

A Quarter of Ice Addicts in Australia Are White Collar Workers
In an article in the Dailymail, rehabilitation company, “The Cabin Addiction Services Group” says an overwhelming number of ice users in rehabilitation belong to the corporate world. Even more shocking is their statement that many of the ice addicts even belong to the health and medical sectors. Ice is an expensive habit to keep, and its users spend at least $500 a day to sustain the habit. Addiction specialists all over Australia confirm the high number of drug abuse problems in white collars, based on the admissions in their rehabilitation centres.
Functional users of ice use it to be more alert, more confident, increase their energy and stamina. Ice, traditionally used by the blue collar workers are now common in finance, management, and IT. And according to the group, ice addicts are able to hide it from their friends, family, and co-workers.
The largest ever seizure of ice was in eastern Melbourne — police found $900 worth of ice, equivalent to 9 million hits.
Straight From the Mouth of a White Collar Heroin User
In 2015 a business analyst from one of the leading trading companies in Australia detailed his 20-year heroin addiction. At the time of writing, he was expecting a large Christmas bonus. That’s on top of earning $100,000 a year. The man admitted to injecting himself with heroin at least once a day and had been an addict since the age of 19. He was still spending his days analysing numbers and advising senior management on business strategies.
In his own words, he was very lucky to have been able to keep his heroin addiction hidden for so long. “I am just a normal person, who happens to have a massive weakness for heroin,” he added.
The director of psychiatry at Royal Brisbane Hospital was astounded to have met such a high-functioning drug abuser, much less a heroin addict. This is clearly not typical, but it highlights how good drug users are at covering up their addiction.

Prescription Drugs – Opioid Misuse on a Steady Rise In Australia
Compared to heroin, prescription pharmaceutical opioids result in more hospitalisations and deaths in Australia. A report by the Australian Institute of Health and Welfare (AIHW) paints a picture of a budding opioid crisis in the country. The number of hospitalisation cases due to the misuse of opioids or overdose rose by 25 percent in the last 10 years.
From 2016 to 2017, there were 5,112 emergency department visits and 9,636 hospital visits due to opioid poisoning alone. According to AIHW spokeswoman, every day there are 150 hospitalisations in Australia due to opioids. Every day in Australia, there are three deaths due to opioid misuse — and the most heavily affected group are Australians that fall between the ages of 35-44. The most common pharmaceutical opioids responsible for deaths were codeine, oxycodone, and morphine.
Monash University student Samantha Lalic analysed the dispensation of opioids under the Pharmaceutical Benefits Scheme (PBS) from 2013 to 2017. She found that 1.9 million Australians begin taking prescribed pharmaceutical opioids every year. Out of the 1.9 million new users, about 50,000 of them end up using pharmaceutical opioids in the long-term, beyond what their doctors prescribe.
Doctors are eager to prescribe pharmaceutical painkillers and their powerfully addictive nature makes patients want to continue taking them long after the need for pain killers has passed. AIHW research data in 2016 shows that 11 percent of Australians admitted to using opioids for non-medical purposes.

White Collar Professionals Reporting To Work Drunk on Alcohol
Out of all the drugs, alcohol is the most accessible. After all, it is perfectly legal. For example, this article highlights the growing number of high functioning alcoholics in Australia. These are well-educated, sophisticated and gainfully employed citizens.
Wastewater Testing Results Highlight The Extent of Drug Use In Australia
Between June and August of last year, researchers from the National Wastewater Drug Monitoring program quietly collected wastewater samples from 58 wastewater stations in the country. The results of the latest wastewater testing were published in February of this year. The sixth annual testing exposes not just the drug habits of Australians according to locality, but also how much Australian’s spend on illegal drugs last year– which is a whopping $9.3 billion.

The drugs detected by the wastewater study include alcohol, ice, amphetamine, MDMA, cannabis, cocaine, oxycodone, and fentanyl. Last year, Australia consumed:
- 9.6 tonnes of ice
- 4 tonnes of cocaine
- 1.1 tonnes of MDMA
- 700 kilograms of heroin
Test results show oxycodone and fentanyl consumption is on a steady rise in the Australian Capital Territory. However, Tasmanians still remain the highest consumer of prescription drugs. Sydney is still cocaine capital with the highest consumption rate of the drug. Ice use in regional Australia grew consistently, with Canberra taking the top spot for residents taking more doses of the drug in a single day. Particularly concerning about this is that ice use is on the rise among young Canberrans.
Furthermore, Victoria takes the place for a state with the highest rates of heroin use, while cannabis use in higher in the regional than metropolitan areas. With MDMA, there is a large variation in the recorded use of the drug. But research shows that it is mostly used for recreational purposes such as in music festivals, where an increase in overdoses cases sparked a national debate. Moreover, alcohol use remains consistent all throughout Australia. It remains one of the most consumed drugs in the country.
The wastewater test results show that there are drug users in every pocket of Australia, both in the regional and metropolitan areas.
Are Your Employees Abusing Drugs and Alcohol?
To sum it up, drug users in our country are intelligent, articulate, employed and have the drive to succeed. A majority are not even aware that they have an addiction, which makes it difficult to address drug abuse.
With the prevalence of drug abuse among white-collar professionals, are you sure that none of your employees are affected? People who work in high-stakes industries are under immense pressure to perform well. Consequently, they may turn to drugs and alcohol to keep their heads above water.
The only way to help a drug-addicted employee and avoid potential disaster is through a drug and alcohol testing program.
The first step is to introduce an enforceable drug testing policy for your company. You are then able to perform mandatory workplace drug testing and address drug use, hopefully in its early stages.
Safework Health can help you secure and safeguard your company and workforce from drug and alcohol abuse through our comprehensive drug testing services.
If you want to know your options, give us a call today.
Learn about MDMA use in Australia and how you can protect your workplace from the affects of MDMA abuse.
Read more
MDMA use is on the rise in Australia. In a shocking statement, even NSW Greens MP Cate Faehrmann recently came out about her own experience using drugs.
In her own words: “I’ve occasionally taken MDMA at dance parties and music festivals. I know journalists, tradies, lawyers, public servants, doctors, police and yes, politicians (most well into their forties), who have done the same.”
If Australians in high and respectable positions have taken MDMA — can you be sure that someone in your staff is not an MDMA user?
Over the past 6 months, there have been five drug-related deaths attributed to MDMA. The spotlight is now on this illicit drug.
What is MDMA?
MDMA or methylenedioxymethamphetamine is a derivative of amphetamine. It is also referred to as ecstasy and Molly, although there are some significant differences.
MDMA vs Ecstasy
A common street name for MDMA is ecstasy.
When Ecstasy boomed in popularity in the early 1980s, it tended to consist of pure MDMA, or sometimes its chemical sister MDA (3,4-methylenedioxyamphetamine). But after MDMA became illegal in the U.S. in 1985, purity began to decrease.
Throughout the 1990s and 2000s, drugs such as cocaine, ketamine and methamphetamine were common adulterants in Ecstasy.
MDMA vs Molly
The term Molly is short for “molecular.” It was given this nickname because this ecstasy drug comes in powder or crystallised form, as opposed to the more traditional pill.
It is commonly marketed as being pure MDMA. But Molly is often the furthest thing from pure MDMA. Synthetic cathinones, also known as “bath salts,” appear to be the most common adulterants or outright replacements.

What makes MDMA particularly dangerous
According to Dr. Judith Perl, a clinical pharmacologist, what makes MDMA particularly dangerous is that the user can never really know the actual MDMA dose they’re taking, much less know what’s in them.
“Often what is sold as MDMA can have other impurities, like MDA (methylenedioxyamphetamine) or PMA (para-Methoxyamphetamine) which can increase the toxicity,” she said.
Dr. Perl also explained that MDMA deaths are mostly due to complications. As the drug greatly impacts the user’s blood pressure, heart rate, and body temperature.
Worryingly, she adds that those who drive under the influence of MDMA are impaired and face the greatest and most fatal risks.
At present, MDMA is more accessible than ever before. Ninety percent of users in the survey describe it as “easy to obtain.” Five or six years ago, only 70 percent of users found it easy to obtain.
Analysis of the Ecstasy and Related Drugs Reporting System (EDRS) reveals that more than one in four people who take stimulants are taking ecstasy on a weekly basis.
The Average MDMA Drug User: Educated and Employed
In an effort to make festivals safer, the National Drug and Alcohol Research Centre interviewed 299 regular users of ecstasy. The average age of participants in the study is 21. And the vast majority were either in school or gainfully employed.
The study shed light on the behavior of MDMA users: they rarely take the drug alone. Nine in ten reported that the last time they used the illicit stimulant, they combined it with alcohol, cannabis, and hallucinogens.
In the AIHW National Drug Strategy Household Survey 2016, MDMA or ecstasy takes the second place in the most commonly used illicit drug by Australians.
Furthermore, the highest rate of illicit drug use (55 percent) is among 30 to 39-year-olds. Next are 40 to 49-year-olds (under 55 percent), then 20 to 29-year-olds (49 percent), lastly are 50 to 59-year-olds (48 percent).
The profile of who uses illicit drugs in Australia is a surprise. It dispels the myth that drug use is prevalent only among the young, uneducated, homeless and unemployed.
In fact, people with post-school qualifications have a 47 percent rate of lifetime drug use. The rate for people with no post-school qualifications is much lower at 34%
In addition, people in the paid workforce have a 51 percent rate of lifetime drug use, compared to 43% among the unemployed.
The results speak for themselves: MDMA drug use is prevalent among adults in the workforce. Imagine these MDMA users driving cars, operating systems, flying planes, and performing surgeries.
It’s a harrowing prospect for a business owner, which is why it is imperative to address MDMA use early on before the stakes get higher.
Long-Term Effects of MDMA Use
Dr. Amy Peacock, the head of NDRAC’s Drug Trend’s project expressed concern over the long-term effects of MDMA use, such as:
- irregular heartbeat
- psychosis
- chronic headaches
- seizures
- kidney failure
- hemorrhaging
- a permanent change in brain function
- memory loss
- depression
For users with pre-existing health conditions, the risks are greater. In fact, most drug deaths that involve MDMA are due to complications and fatal reactions.

The MDMA Drug and Its Impact on the Australian Workplace
Having an MDMA user on staff comes with serious risks. Drugs, along with alcohol, cost Australian businesses an estimated $6 billion per year in lost productivity.
An estimated 2.5 million days are lost due to drug and alcohol use, costing Australian businesses $680 million. The staggering figures do not include the safety issues that come with having a drug using employee.
Workers in safety-sensitive industries who use MDMA are putting not only themselves in danger but also others. While the effects of ecstasy last 24 hours, residual effects can last for days. So if an employee takes ecstasy over the weekend, he or she will be experiencing the aftereffects while at work.
The stigma surrounding illicit drug use and a lack of a workplace drug policy is a potentially lethal combination. By the time MDMA use is found out, it’s usually too late.
An employee who takes MDMA over the weekend will usually carry over the aftereffects into work. A user coming down on ecstasy will suffer from the following:
- Anxiety
- Paranoia
- Impaired judgment
- Lack of focus
- Poor concentration
- Blurred vision
- Muscle tension
As an employer, you are responsible for any accidents at work that involve ecstasy use. In effect, you are legally bound to pay for Workman’s Compensation claims.
Things could get worse if an employee files a case against negligence in court. And the bills from the litigation process can easily pile up in a short span of time.
The good news is, you can proactively protect your business and employees from the dangers of MDMA use.
Testing For Ecstasy At Work
You do not want ecstasy users in safety-sensitive jobs where they operate heavy equipment or transport people or goods.
With a workplace drug program that includes testing for ecstasy and MDMA, you’ll find out who among your employees take ecstasy. After which, you can take the necessary steps as stated in the workplace drug policy. This is the best thing that you can do to address ecstasy use at work.
Safework Health offer safe, hygienic, and discreet onsite testing for ecstasy so there is minimal disruption to your workforce. We can also help you develop a comprehensive MDMA safe workplace program that includes education programs that deter drug use among your employees.
If you want to find out more about developing a drug policy or ecstasy testing, please get in touch with us today. All our discussions are strictly confidential.
Find out how you can tell if your co-worker is using illicit drugs.
Read more
Did you know that Australia loses an estimated $6 billion per year in productivity due to alcohol and drug abuse in the workplace?
This according to research published by the Alcohol and Drug Foundation of Australia.
If you think that this is something that you shouldn’t worry about — think again.
According to the Alcohol and Drug Foundation, one in ten workers have had negative experiences with co-workers taking drugs. These include being prevented from doing their job, always covering for their co-worker, and experiencing minor to major accidents at work.
Every worker should still feel safe in their working environment. Rampant drug use in the workplace robs employees of the chance to feel safe, and thereby affects their productivity.
Is my co-worker using illicit drugs?
Things to look out for are:
- Frequent absences
- A negative disposition or having a bleak outlook in life
- Lack of focus and productivity
- Loss of interest in daily activities
- The need to sleep at work
- Not eating well or a lack of appetite
- A frequency of accidents and mishaps
- Requesting for worker’s compensation much more than the average employee
- Involvement in workplace fatalities
Look for the physical signs of drug abuse
Some of the signs and symptoms of drug abuse are:
- Bloodshot eyes
- Dilated pupils
- Sudden and drastic weight gain or weight loss
- A gaunt and tired appearance
- Slurred speech patterns
- Highly irritable
- Frequent drowsiness
- Changes in personal grooming habits; no regard for hygiene
- Unusual body odour
- Trembling
- Excessive sweating
If your co-worker has more than two of the signs above, you have every right to be worried.
Sometimes, a colleague’s empathy and concern go a long way. Remember that you are dealing with someone’s livelihood and reputation. This is a delicate matter that has to be dealt with using utmost confidentiality.
How to handle your suspicion?
1. Talk to our co-worker
If you choose to talk to your colleague, avoid being confrontational. You do not know what your co-worker is going through. There are many reasons why a person could show the above symptoms.
It’s best to start by asking them how they are and if they’re okay.
Always, always, come from a place of compassion and try to empathise with your co-worker. Make sure he or she knows that you are concerned for their well-being.
It could be that your co-worker has developed a poor way of handling stress and pressure. It could also be that he or she is having a very difficult time at home.
While a drug user may not admit to having a problem, it won’t hurt to reach out.
After speaking with your co-worker, it is probably time to alert human resources to the situation.

2. Talk to Human Resources
This is an unavoidable step to take when it comes to addressing your co-workers illicit drug use.
Drug addictions are a very serious and delicate matter. They are to be dealt with by a professional or trained personnel.
Human Resource personnel are well-trained to deal with a drug using employee. Chances are, they’ve handled this type of situation before and will know what to do.
3. Talk to their Supervisor
If reporting to Human Resources fails to yield any results, talk to your supervisor.
You should also refer to your company’s drug and alcohol policy. Ideally, there should be written guidelines for handling a drug using employee.
The best workplace policies include drug testing and training and education as part of their program.
In the event that your company does not have a workplace alcohol and drug policy, suggest to create an immediate action plan to assess the situation.
Sitting back and minding your own business is not the attitude you should be taking when dealing with a possible drug addicted colleague.
Every employee has a responsibility to maintain a positive and safe workplace where you all can thrive. Always take it upon yourself to take the necessary steps to prevent any untoward incidents at work.
Learn More
Contact us today for information on how we can keep your workplace safe from drug use and abuse.
Discover the workplace drug testing implications for legal cannabis in Australia.
Read more
The Federal Greens party in Australia announced that they would push to make cannabis or marijuana legal for all people over 18 years old.
This continues a topic of conversation that has been occurring in Australia for several years. A case made more pressing given the recent legalisation of cannabis in several states in the USA, and the recent legal changes to the status of medicinal cannabis.
Safework Health constantly monitors the advances in science and technology as well as the policy and regulatory framework for workplace drug testing. We always do our best to educate, inform and stimulate discussion in this dynamic area.
This commentary covers our point of view on an article published by the ABC by political reporters Matthew Doran and Lucy Barbour. It is titled Greens announce plan to legalise cannabis to take it ‘out of the hands of criminals and dealers’.
So, what would be the implications for workplace drug testing?
On one level, very little. Given that both Australian Standards (AS/NZS4308 and AS4760) require Cannabis to be tested – specifically the psychoactive component THC (tetrahydrocannabinol).
Both standards already mandate testing for a mix of drugs such as Cocaine and Methamphetamine, which are clearly illegal. The same goes for prescription-only drugs such as Opiates and Benzodiazepines.
So any drug and alcohol policy that requires adherence to these standards would have to continue to drug test for Cannabis regardless of any change in the legality of the drug.
Alcohol isn’t illegal either. Couldn’t we treat it the same as that?
But what of the moral argument that companies will be testing for – and potentially penalising workers for – a drug which would be legal to consume?
Well, currently almost all companies already do this for Alcohol. It is very rare to find a company that would allow workers to consume excessive amounts of alcohol on site and still declare themselves fit for work. Most especially in a safety-sensitive environment.
But of course, we have good tools for measuring the amount of alcohol present in a person’s body. The usual method being via a handheld breath alcohol detector.
So employers and employees can determine the maximum “safe” level of alcohol intoxication depending on the role (eg zero, 0.02% or 0.05% BAC).
So what’s the “safe” level of cannabis in regards to safety?
Short of a blood test, there is no truly accurate way of determining how much THC an individual has in their system at any given time. There is also the problem that THC and ethanol have very different characteristics in terms of their performance effects.
Small amounts of cannabis intoxication have similar results on safety tests as do much larger doses. This is true in the case of a simulated driving performance.
Subjects show substantial negative performance at very low doses. But they do not perform a great deal worse as the level of cannabis present increases.
Alcohol is very different in this regard though. An individual can display very few effects at low doses (such as 0.02% BAC). But performance gets progressively worse as their alcohol level increases.
So it’s not really a valid comparison, at least as far as the science of the drugs themselves is concerned.

What about medicinal cannabis? That’s already legal
It’s quite true that cannabis has been available by prescription in Australia for some months now. Most companies have dealt with this change by applying exactly the same criteria as they do with other prescription drugs. Any individual who has a confirmed positive result for, say a Benzodiazepines drug test, must produce their prescription for that drug.
Ideally, the employee will have also had a conversation with their prescribing GP, medical specialist or Pharmacist about the potential safety consequences of taking this medication. And if there is any further doubt, a company doctor or Occupational Physician can provide further input and advice.
Medical cannabis can be treated in exactly the same manner.
It seems unlikely in the short term that there will be any substantial changes to the legal status of Cannabis or any other currently illegal drugs.
Learn More
Contact us today for information on how we can keep your workplace safe from cannabis use and abuse.