We are pleased to announce Matthew Holt has been appointed as Safework Health’s Managing Director.
Read more
Effective February 9, 2024, Mal Beacham, the Managing Director and a founder of Safework Health, has transitioned from his role. We extend our best wishes to Mal for his future endeavours and appreciate the contributions he has made to the company.
On a positive note, we are pleased to announce that Matthew Holt will be assuming Mal’s role and responsibilities as the Managing Director of Safework Health, effective immediately.
Matt has been a valuable member of Safework Health’s leadership team for several years, demonstrating a solid understanding of the business and fostering strong relationships with key customers and staff.
The Safework Health board fully supports Matt, and we look forward to working closely with him in this new role.
Our Brisbane clinic is now accredited to offer Coal Board Medicals. Book now!
Read more
Safework Health is thrilled to announce our Brisbane clinic is now accredited to provide Qld Coal Board Medicals. This accreditation marks a significant milestone in our commitment to ensuring the health and safety of workers in the coal mining industry.

Comprehensive Occupational Health Services
At our clinic, we understand the importance of comprehensive medical assessments for various industries. That’s why, besides Coal Board Medicals, we offer a range of other essential services tailored to meet the needs of different sectors.
These services include Pre-employment Medicals, Mining Medicals, MMQ Medicals, OGUK Medicals, AMSA Medicals, Rail Medicals, CASA Medicals, Driver Medicals, and Drug and Alcohol Testing.

Convenient and Accessible Location
Located in the Brisbane suburb of Murarrie, our clinic offers convenient access to individuals and businesses in the surrounding areas.
Whether you are a coal mine worker needing a mandatory Coal Board Medical or an employer seeking comprehensive pre-employment screenings for your workforce, our clinic provides a central and easily accessible location for all your workplace health needs.

Helping You Hire The Right Person Quickly
When you choose Safework Health, you can trust that you are in capable hands. Our experienced occupational health professionals are well-versed in industry-specific health assessments and are committed to delivering accurate and reliable results quickly.
- Fast and accurate results – Enabling you to make informed decisions
- Flexible bookings – Same-day appointments available
- Customised service – Assessment tailored to you
- Services performed in-house – We employ a national team of qualified and friendly doctors and nurses
Book Now
For appointments or enquiries about our services, please contact us today.
Explore AS/NZS 4308:2023, reshaping workplace drug testing. Uncover vital changes impacting your program for effective compliance.
Read more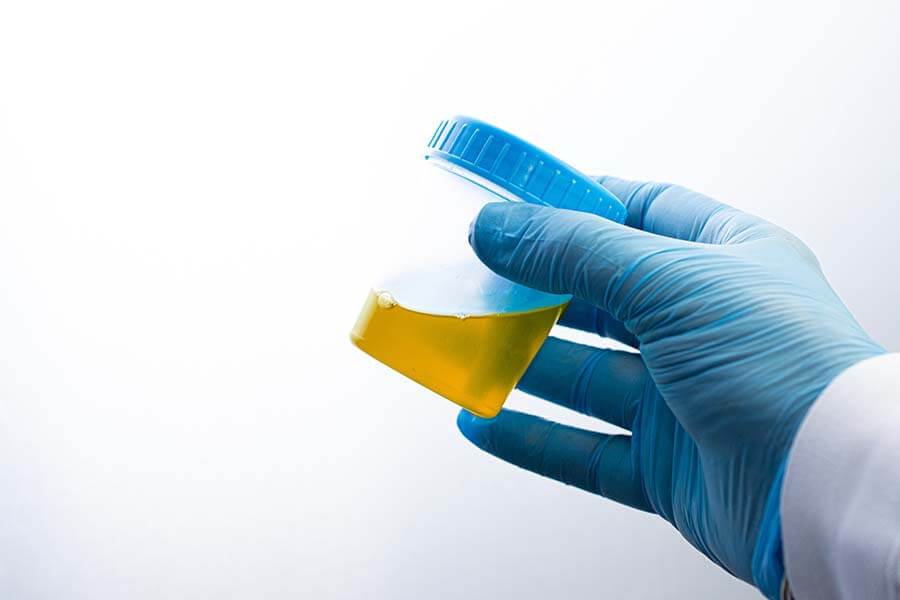
Introducing the latest benchmark in workplace urine drug testing: AS/NZS 4308:2023. This new standard marks a significant departure from its predecessor, AS/NZS 4308:2008, bringing about key changes that have implications for your workplace drug testing program.
Delve into the details to better understand the modifications and their impact on your workplace.
About AS/NZS 4308:2023
AS/NZS 4308:2023 sets the benchmark for procedures concerning urine specimen collection, storage, handling, onsite drug screening tests, and dispatch to a laboratory. It’s a vital resource for maintaining best practices in drug testing.
Unveiling 3 Key Shifts in Workplace Drug Testing
- The first key change is a DECREASE in the screening cut-off for cocaine metabolites, from 300 ug/L down to 150 ug/L, and a corresponding drop in the confirmatory cut-off from 150 ug/L down to 100 ug/L. This should result in more detections on-site, along with confirmatory testing being more likely to match the initial screening result.
- The second key change is a DECREASE in the confirmatory cut-off levels for Benzodiazepine metabolites, from 200 ug/L down to 100 ug/L. This will reduce the likelihood of a non-negative on-site screen returning a confirmed negative confirmation due to a mixture of metabolites being present in the urine with no individual component over 200 ug/L. Screening cut-offs for Benzodiazepines remain at 200 ug/L.
- The third key change is allowing laboratories to report parent/metabolite drug(s) that are detected below the cut-off, but between the laboratories limits of quantitation (LOQ) and the cut-off, where another drug/metabolite has been detected above the cut-off. For example, when amphetamine is detected in a sample and a low level of Methamphetamine is present, that Methamphetamine result will additionally be reported to aid in the interpretation of results.
Other minor changes/additions include:
- Expanded reference to Informed Consent in relation to scope of testing.
- Centralised QC testing of devices at the main storage site, as opposed to on -site prior to testing.
- Allowances for Liquid Chromatography Mass Spectrometry (LCMS) based screening of drugs, with cut-offs as per confirmatory methods.
- Oxycodone has specified cutoffs for screening and confirmation, but is not included in the main testing panel.
Cut-Off Levels for THC Remain Unchanged
There are no changes to the testing process for THC in the urine standard. All cut-offs remain the same.
Implementation Timeline
AS/NZS 4308:2023 also introduces a crossover period for 3 years where both standards are in effect, allowing manufacturers, laboratories, and collection agencies to implement changes when devices, laboratory procedures and processes have been updated to meet the new requirements.
Discover More
A Safework Health representative is available to discuss the upcoming changes and the proposed timeline for implementation. Contact our team today!
Pathology Asia has joined the Global Diagnostics Network – a worldwide network of diagnostic laboratories.
Read moreWe are pleased to announce Pathology Asia’s inclusion as a member of the Global Diagnostics Network (GDN), a strategic working group of diagnostic laboratories from around the world. Pathology Asia was introduced to this globe-spanning community in July 2023.
Pathology Asia’s membership in the GDN reinforces its commitment to ensuring that healthcare professionals are well-informed when making choices that will shape medical decisions and health diagnoses. It also furthers their goal to become a fully integrated digital healthcare organisation.
About the Global Diagnostics Network
The GDN was conceptualised by US-based Quest Diagnostics as a worldwide community of leading healthcare companies. This worldwide network was designed to develop collaborations among the world’s leading healthcare companies to address the growing need for advanced diagnostic testing and high-quality healthcare services.
Presently, the Network has a presence in countries with two-thirds of the world’s population and over 90% of the global pharmaceutical market. Its members include Quest Diagnostics, Al Borg Medical Laboratories, Apollo Health & Lifestyle, Dasa, GC Labs, Healius, Lifelabs, LSI Medience , KingMed Diagnostics, Pathology Asia, Strand Life Sciences, and SYNLAB.
Proud Member of the Pathology Asia Group
Safework Health has been a member of the Pathology Asia group since 2019. The Group is one of the largest and fastest-growing diagnostics groups in the region and comprises leading diagnostic laboratories across Southeast Asia and Australia.
View the Q&A from our Drug and Alcohol Policy Development Workshop.
Read more
During our Drug and Alcohol Policy Development Workshop held on 29 November 2023, numerous questions were asked, some of which we did not have time to answer during the session. Below are all the questions asked, along with our responses.
Should you have any additional questions, please don’t hesitate to reach out to us at [email protected] or 1300 795 227.
Webinar Q&A
Performing the testing of wastewater, is that something you can carry out on all sites? Is it an easy test to complete?
Wastewater testing can be performed effectively at any site. All that is required is to get access to the effluent outflow or the wastewater holding tanks for sampling. If required, Safework Health can send our staff to your sites and assess what needs to be done for testing and advise on the optimum testing regime tailored to your needs. Wastewater testing requires as a minimum that the number of staff at the site at the time of testing be made available. The effluent flow rate would be helpful but is not critical, as it can be approximated from the staff numbers assuming the average number of toilet visits and the average Australian toilet flush volume. Each sampling episode is easily done by taking ~300mL of wastewater from the effluent stream. Reports will be available within 7 working days of receipt of the sample.
Do we need to notify the employees that we are going to conduct wastewater testing?
There is no requirement – either legally or by custom, in Australia or internationally – to inform a site that wastewater testing is being or is planned to be performed. Wastewater testing is a whole-site testing procedure and does not impact the individual workers. Results reveal the magnitude of drug use at a site collectively and cannot identify the individual workers involved, so no case can be made for generally informing a site that testing will take place.
Do you see a time when we will have standards for hair testing?
It is generally believed the European SoHT (Society of Hair Testing) recommendations will be adopted as the international standard for hair testing by the EU over the next 2 to 3 years – specifically the 2022 Consensus on Hair Testing. The current delay is due to problems reconciling French guidelines with German practice. Once the EU has given its imprimatur, the US and Australia will follow suit to comply with international best practice guidelines.
Can you share that evidence base for >1 per year drug and alcohol testing programs reducing accidents by X%?
In progress. The review of the literature will be made available on 12 December 2023.
Do the laboratory test results reflect how long ago the worker is likely to have taken THC? Namely, can the result be converted into a rough timeline of when the THC was used?
No exact figure can be given. Urinary THC (provided the donor’s physiological details are supplied) may potentially supply the most accurate (albeit rough) estimate.
The oral fluid detection window for THC is roughly 8-12 hrs for standard doses of medicinal cannabis, ~ 12-18 hours for a NIDA-standard low dose 5mg THC cigarette, 18-24+hrs for a NIDA moderate dose 10mg THC cigarette. By use of the detection window a crude estimate of the maximum time since use can be made.
Urine detection windows are more complex. THC is a lipid-soluble molecule which partitions into the body fat. The more frequent the use of cannabis, and/or the more adipose tissue a donor has, the longer the detection window for THC – ranging from 3 to 5 days for a standard NIDA cigarette in a donor with normal BMI to 7 days for an obese donor with a BMI > 28.
By factoring in the height/weight and age of the donor and the stated frequency of use, a rough estimate of the time since use (i.e., more than ‘x’ hours but less than ‘y’ hours before collection) can be made for a range of THC doses, as well as determining whether a particular urinary THC level is consistent with the donor’s stated dosage and declared time since use. It should be noted these estimates are rough and not exact and that, while oral fluid THC correlates well with THC-associated impairment (if it’s not detected, the donor’s not affected), urinary THC levels do not correlate with impairment.
Watch The Webinar
Did you miss the webinar? Don’t worry, you can watch a recording of the webinar here.
Meet Maree, a dedicated Occupational Health Nurse in our Brisbane clinic.
Read moreMeet Maree, an Occupational Health Nurse at our Brisbane clinic. With 20+ years of nursing experience, Maree has found immense fulfilment in her role here since joining Safework Health in March 2023.
When not at work, Maree is all about staying active with reformer Pilates, running, paddle boarding, and kayaking. She also enjoys family time with her three beautiful grandchildren.
Meet Our Growing Team
Find out more about Safework Health’s national occupational health team.
Join our webinar and discover the keys to crafting a customised drug and alcohol policy that perfectly suits your business. Register now!
Read more
Are you concerned about workplace substance abuse and the legal responsibilities it entails? We invite you to our upcoming webinar, where we’ll equip you with essential insights and tools to create a comprehensive Drug and Alcohol Policy tailored to your business’s unique needs.
Date: Wednesday, 29 November
Time: 1 PM AEDT
The event will be made available on-demand to all registrants, so even if you can’t make the live show, please register.
In this webinar, we will explore:
- Legislative Requirements and Fiduciary Duty-of-Care: We’ll dive into the legal obligations and fiduciary responsibilities related to workplace drug testing.
- Assessing Your Workplace Needs: Learn how to assess your workplace to determine the extent of substance abuse issues and identify specific needs.
- Developing a Written Policy: We’ll provide guidelines and a template to help you create a robust and effective drug-free workplace policy.
- Implementing Drug Testing: Discover how to choose the right test mix and testing strategy to suit your business’s requirements, including considerations for frequency and types of testing.
- Education & Training: Explore the importance of providing education and training for employees and additional training for supervisors and other relevant staff.
- Employee Assistance Program (EAP): Gain insights into setting up and assessing your EAP to support employees dealing with substance abuse issues.

Meet Our Webinar Speaker
Dr Phil Tynan, National Chief Toxicologist
Dr Tynan, a renowned Toxicologist, and retired Clinical Biochemist Pathologist, offers a wealth of industry experience. He specialises in substance abuse testing, supports Safework Health in developing new assays and procedures, and provides expert advice to clients. With publications in peer-reviewed journals, Dr Tynan is available for result consultation, expert witness testimony, and court appearances.
Explore the impact of fentanyl and oxycodone in Australia, uncover evolving trends, and discover workplace testing methods.
Read more
Fentanyl and oxycodone, the key players in the opioid epidemic sweeping across the United States, have begun to reshape the landscape of opioid use in Australia. While usage rates here remain lower than in the US, recent studies reveal a shift in opioid consumption patterns.
In this engaging article, we delve into the world of fentanyl and oxycodone, exploring their impact on Australia, tracing the evolving usage trends, and shedding light on effective workplace testing methods for detecting their presence.
Fentanyl vs Oxycodone
Fentanyl and oxycodone are powerful and highly addictive opioids commonly used for pain management.
What is Fentanyl?
Fentanyl is a synthetic opiate drug that is 80 to 100 times more powerful than morphine.
It is used medically as an intravenous anaesthetic and analgesic. However, it is most often encountered as a transdermal (skin) patch to relieve long-term pain, or to supply relief to cancer patients and the elderly. The drug is often misleadingly marketed as ‘safe’.
These patches are frequently discarded when they are around two-thirds used as the quality of pain relief tends to drop over time. Unfortunately, these ‘used’ patches can be reused by addicts when they extract the fentanyl gel. This practice is called ‘dumpster diving’ because they often search for old patches in the garbage. They then distil the pure drug from the patches and often recrystallise the drug to form “Rock.” Fentanyl distillates can be smoked, or the patches can be used directly – either being pasted on the body or chewed.
Traditionally fentanyl powder is often mixed with low-quality heroin. Heroin supplies from Central Asia are drying up. This is pushing users to experiment with fentanyl.
Additionally, increasing amounts of fentanyl are being imported into Australia. Just last year, the Federal Police in Melbourne seized a shipment of fentanyl equivalent to 5 million individual doses.
What is Oxycodone?
Like fentanyl, oxycodone is a synthetic opiate often sold as Oxycontin or Endone which, when taken by mouth, is one-and-a-half times more potent than morphine.
Medically, it is used for managing moderate-to-severe acute or chronic pain and is normally sold as a controlled-release tablet to be taken every 12 hours. As with all opioids, oxycodone induces euphoria and is addictive.
Oxycodone is one of the most abused pharmaceutical drugs in the US and is significantly abused in Australia, although not (as yet!) at levels approaching those in the US.
Once a person becomes physically dependent on oxycodone, they experience strong cravings for the drug, leading to continued use despite the ongoing physical harm. They are also at risk of suffering severe withdrawal symptoms, which can include panic attacks, nausea, muscle pain, insomnia, and flu-like symptoms.
Overdoses can easily be fatal. When not fatal, they can cause spinal cord infarction and ischaemic brain damage that resembles a bad stroke. Oxycodone also interacts badly with many other prescribed drugs – especially some anti-HIV medications – which can substantially slow the rate of clearance of the drug from the body.
Combining Opioids With Stimulants
Oxycodone and fentanyl are now being increasingly used in combination with stimulants – especially of the amphetamine class (which includes Meth).
There is a long history of people combining opioids with stimulants, such as ‘goofballs’ combining methamphetamine with heroin and ‘speedballs’ which are a heroin plus cocaine mixture. Australia already has a widespread Meth problem, and the number of cases where opioids were combined with Meth is rising.
Oxycodone and Fentanyl Usage Trends in Australia
There is a growing opioid abuse culture in Australia.
Even in 2008, the National Drug & Alcohol Research Centre reported that 91% of injecting drug users in Australia report having used Oxycodone. 23% admitted to using it in the last 6 months.
Fentanyl use has been rising in Australia, especially over the last 4 years – most notably on the Sunshine Coast in Queensland. Programs to stop fentanyl use have been only partly successful as addicts often switch over to oxycodone.
Oxycodone and fentanyl use in Australia is substantially higher in regional areas than in urban and capital areas, but the overall use rate is significant in both areas.
Worksite drug testing has shown that the use of these drugs varies substantially over the week. In remote sites, importation may occur only on specific days – which is then reflected in higher capture rates over the next 24-48 hours.
Cracking down on one opioid – such as oxycodone – only appears to encourage users to switch to another opioid: specifically, fentanyl. This was seen in the closing years of the last decade in Queensland where a crackdown on oxycodone led to a rise in fentanyl abuse.
Surging Popularity of Fentanyl and Oxycodone: Examining the Pros and Cons
What is the danger if oxycodone and fentanyl use are on the rise?
Both fentanyl and oxycodone carry a high risk of making users dependent on the drugs, and both have what is called a narrow therapeutic window: a dose sufficient to bring on a high is not much less than the dose required to give a potentially lethal overdose.
The appeal of fentanyl and oxycodone is that the drugs are pharmaceutical – so they have a high purity, and users are less worried about contamination. The drugs are highly potent – ‘more bangs for the buck’ – and because of their rapid uptake cause a ‘quick high’ (especially fentanyl).
The advantage from a medical perspective is that fentanyl can be taken when a patient has an impaired liver, to treat neuropathic pain, and the patches can be used when a patient is nauseous, vomiting or has difficulty swallowing. For the user, the big attraction is that fentanyl is the fastest-acting opioid available.
Fentanyl is cheap – so it is a popular opioid for abuse. Unfortunately, it also has the most prolonged respiratory depression (suppression of the breathing reflex) of any opioid – which arguably makes it the most lethal.
Workplace Drug Testing: Detecting Oxycodone and Fentanyl Use
Common workplace drug testing methods include:
- Urine Drug Testing – Oxycodone and fentanyl can be detected in a specifically requested assay in urine. Urine is the superior sample for both drugs, as the detection window is much greater than oral fluid – up to 4 days.
- Oral Fluid Drug Testing – Oxycodone is included in routine oral fluid screening tests, unlike fentanyl which is not included in these tests. The detection window for oral fluid is 36 hours.
- Wastewater Drug Testing – Wastewater drug testing is the best way to get a snapshot of the extent of actual opioid use at a workplace but should include weekend coverage as use varies greatly day-to-day.
Safework Health: A Leader In Workplace Drug Testing
Safework Health stands out as one of the select few laboratories in Australia capable of conducting urine testing specifically for oxycodone and fentanyl.
Plus, we offer a verified onsite urine drug screening device that can detect Fentanyl, Oxycodone and Ketamine.
Feel free to reach out to us today for a discreet and confidential consultation.

Meet The Author
Dr Phil Tynan, National Toxicologist
Dr Tynan, a distinguished Toxicologist and a retired Clinical Biochemist Pathologist, brings a wealth of industry knowledge and experience. He is considered an expert in testing for substances of abuse.
Dr Tynan primarily supports Safework Health in developing new drug assays and procedures. He also offers guidance to clients and expert clinical advice as needed.
Dr Tynan is a published toxicologist in internationally peer-reviewed journals and is available to provide advice and expert opinion regarding results, expert witness testimony and appearances at courts and tribunal hearings.
Learn what isocyanates are, health hazards, and the importance of health monitoring programs.
Read more
Isocyanates are highly reactive compounds used in industries like adhesives and coatings. Exposure can lead to health problems such as asthma and skin sensitisation.
To help keep your workers safe and healthy, we have created a comprehensive guide. This guide covers essential information about isocyanates, including what they are, the health hazards associated with their exposure, and the importance of implementing a health monitoring program.
What Are Isocyanates?
Isocyanates are a group of highly reactive organic compounds used in the manufacture of:
- adhesives and glues
- coatings lacquers and varnishes
- spray paints
- elastomers and foams
- floor / roof screeding
- hardwearing plastics
- medical dressings
Isocyanates are toxic until they react with other chemicals to form the hardened or ‘cured ‘polyurethane product. Fully-cured polyurethanes are non-toxic, unless they are heated or abraded, which makes them give off isocyanates and other toxic substances.

Understanding Isocyanate Exposure
Isocyanates can enter the lungs when workers inhale isocyanate vapours, mists or aerosols. They can also be absorbed when a worker’s skin is exposed to liquids, resins, or droplets. Even workers who don’t handle isocyanates directly, but work near others who are using isocyanates, can still be exposed.
Isocyanate exposure can occur throughout the manufacturing process, from initial surface application to cutting or curing.
Exposure is common in many industries including painting, printing, automotive manufacture, construction, furniture production, and mining.
Isocyanates Health Effects
Isocyanate exposure is associated with numerous health problems. Exposure can cause asthma, skin sensitisation, skin or mucous membrane irritation, and, rarely, a lung reaction called hypersensitivity pneumonitis.
Occupational Asthma
They are one of the leading causes of occupational asthma in Australia. The condition commonly presents as:
- wheezing
- chest tightness and shortness of breath
- cough
The symptoms can occur at work, or much later after work, and the asthma can be made much worse by repeated exposure.
Once a worker has been sensitised, even very low-level exposures might produce a potentially life-threatening asthma attack, which may end their career. Exposure to isocyanate aerosols can lead to hypersensitisation which can give rise to ‘bagpipe lung’ (also known as extrinsic allergic alveolitis or hypersensitivity pneumonitis).
Skin Sensitisation
Sensitisation by skin contact can cause allergies that can affect both the skin and/or the lungs. Acute exposure to these chemicals can cause irritation to the eyes, skin, and mucous membranes of the nose and the throat, occasionally accompanied by headaches and itching. Sensitisation can occur at isocyanate concentrations lower than those that may give rise to irritation.
Potentially Cancer-Causing
Most isocyanates are not carcinogens – the exception is TDI (toluene diisocyanate) which has been found to cause cancer in some laboratory animals (although it has never actually been demonstrated in humans). Isocyanates are not associated with human fertility or pregnancy problems nor with abnormalities of foetal development.
Exposure Testing and Control Measures
To safeguard workers’ health and minimise the risks associated with exposure, control measures and biological monitoring programs are essential.
Control Measures
Since isocyanates can act as skin and respiratory sensitisers, and to control the risk of future health issues in the workplace, exposure to isocyanates should be kept as low as reasonably practicable.
If adequate control measures are in place – such as closed ventilation systems (spray booths, enclosed moulding machines), air-fed respiratory protection and personal protective clothing/gloves – these conditions, and episodes of isocyanate exposure, are easily preventable.
Biological Monitoring Program
Isocyanate Biological Monitoring (BM) is especially necessary for workers involved with:
- motor vehicle repair paint use
- foam blowing
- hard polyurethane manufacture
- glues and adhesives
- floor screeding
- underground mining.
BM is a simple and cost-effective way to check that workplace control measures are sufficient, being effectively applied and exposure is being adequately controlled.
BM assesses worker exposure to isocyanates, confirms control measures, and prevents health risks. While not a diagnostic tool for isocyanate-related conditions, it helps identify occupational exposure when symptoms arise. BM also gauges skin absorption, especially with glove use. It’s user-friendly, providing personalised results to promote better work habits.
BM aggregates all routes of exposure, inhalation, skin absorption and ingestion, so a result cannot identify the actual source/route of exposure. It will, however, show the need for corrective action to be taken.
Safe Work Australia’s Guidelines for Isocyanate Exposure Monitoring
Safe Work Australia recommends that Biological Monitoring programs for workers using or exposed to isocyanates should include:
- Initial baseline BM upon the commencing employment
- Periodic BM review, generally performed after 6 weeks of commencement (of isocyanate exposure)
- Regular 6-monthly BM every six months. If after 12 months, no adverse health issues are reported this should then switch to annual testing
- Terminal BM performed at the end/termination of the period of isocyanate exposure.
How Is Isocyanate Exposure Testing Performed?
A post-exposure urine sample should be taken, ideally within an hour of the end of exposure, especially for those tasks involving:
i) heating of polyurethane
ii) use of:
- HDI (hexamethylene diisocyanate, used in two-pack spray paints)
- TDI (toluene diisocyanate, used in adhesives and foam blowing)
This is recommended as the above-mentioned isocyanates are all rapidly excreted.
End-of-shift testing should be performed with:
i) Encountering abrasion of polyurethane
ii) Exposure to MDI (methyl phenylene diisocyanate)
If significant skin exposure is a possibility, pre-shift next-day samples should also be considered (due to the delayed absorption through the skin).
BM samples mostly reflect that day’s exposure (reflecting the short half-life of excretion), and generally do not illuminate long-term exposure. For this reason, it is recommended that several samples are taken initially to ensure that ‘normal practice’ is captured.
The urine samples should be sent ideally the same day or the next day to Safework Health for analysis. If shipping is delayed, samples should be stored frozen, if possible, prior to despatch.
How do you interpret results?
Interpretation of results requires an appreciation of the work practices, tasks and controls used by an individual worker on the day of sampling.
Results will fit one of three broad categories:
- No detection — with no evidence of exposure to the requested isocyanates (no further action required and repeat testing in 1 year)
- Low-level exposure — meaning that exposure was detected but the levels were within the BMGV (control measures and their use should be checked but repeat testing is not required immediately; the result may be due to intermittent behaviours, such a visor-flipping, if the investigation shows no systematic concerns); and
- Exposure exceeds the BMGV — this requires action be taken to check the control measures and their use and to resample workers once any issues have been resolved (if results remain elevated, further investigation is required but workers do not need to be removed from tasks). Where work practices or exposure controls are significantly altered then retesting should be considered to ensure that exposure levels have not increased as a result.
Safework Health’s Biological Monitoring Service
Safework Health’s NATA accredited isocyanate urine testing service can detect your workers’ exposure to this harmful chemical. We offer a rapid 5-day turnaround for results, an accurate and cost-effective testing method, and national coverage.
Contact our friendly team today to find out how we can keep your workers safe and healthy.


